A Columbia University study has found that adversity early in life is associated with increased gastrointestinal symptoms that may affect children’s brains and behavior as they mature.
“It is too early to say anything conclusive, but our study indicates that adversity-associated changes in the gut microbiome are related to brain function, including differences in the regions of the brain associated with emotional processing,” said Nim Tottenham, a professor of psychology at Columbia and senior author on the study.
The study, “Mind and Gut: Associations Between Mood and Gastrointestinal Distress in Children Exposed to Diversity,” was published online March 28 in the journal Development and Psychopathology.
“One common reason children show up at doctors’ offices is intestinal complaints,” said Tottenham, who is an expert in emotional development. “Our findings indicate that gastrointestinal symptoms in young children could be a red flag for future emotional health problems.”
Scientists have long noted the strong connection between the gut and brain.
A history of trauma or abuse, even in the second through sixth weeks after birth, is associated with a higher risk of irritable bowel syndrome and more than one-third of mental-illness diagnoses in one’s lifetime, according to previous research. This study was designed to determine when childhood adversity begins to affect the gastrointestinal system.
“The role of trauma in increasing vulnerability to both gastrointestinal and mental health symptoms is well established in adults but rarely studied in childhood,” lead author Bridget Callaghan, a post-doctoral research fellow in Columbia’s psychology department, said in a released statement. In addition, animal studies have demonstrated that adversity-induced changes in the gut microbiome—the community of bacteria in the body that regulates everything from digestion to immune system function—influence neurological development, but no human studies have done so, she said.
“Our study is among the first to link disruption of a child’s gastrointestinal microbiome triggered by early life adversity with brain activity in regions associated with emotional health,” Callaghan said.
The researchers focused on development in children who experienced extreme psychosocial deprivation due to foster or institutional care before international adoption. Separation of a child from a parent is known to be a powerful predictor of mental health issues in humans. That experience, when modeled in rodents, induces fear and anxiety, hinders neurodevelopment and alters microbial communities across the lifespan.
The researchers drew upon data from 115 children adopted from orphanages or foster care on or before they were 2 years old and from 229 children raised by a biological caregiver. The children with past caregiving disruptions showed higher levels of symptoms that included stomach aches, constipation, vomiting, and nausea.
From that sample of adoptees, the researchers then selected eight participants, ages 7 to 13, from the adversity exposed group and another eight who’d been raised by their biological parents. Tottenham and Callaghan collected behavioral information, stool samples and brain images from all the children. They used gene sequencing to identify the microbes present in the stool samples and examined the abundance and diversity of bacteria in each participant’s fecal matter.
The children with a history of early caregiving disruptions had distinctly different gut microbiomes from those raised with biological caregivers from birth. Brain scans of all the children also showed that brain activity patterns were correlated with certain bacteria. For example, the children raised by biological parents had increased gut microbiome diversity, which is linked to the prefrontal cortex, a region of the brain known to help regulate emotions.
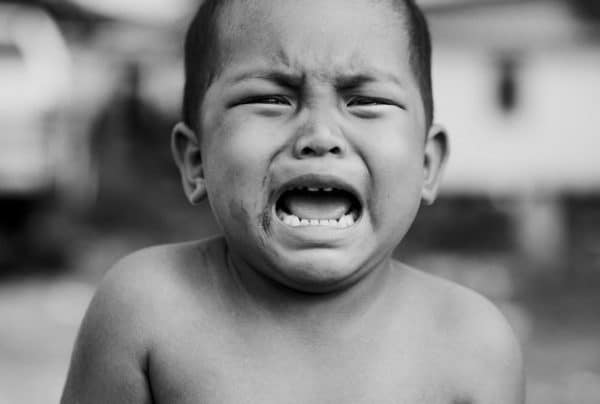
“We observed that early adversity was associated with gastrointestinal symptoms in youth aged 3-18 years (with the largest effects observed in late childhood),” the authors wrote. They also found that adverse caregiving experiences in the earliest days of life alters the gut’s biome; that variation affects how the brain’s emotion networks develop.
“The fact that early experiences of caregiving adversity increase the risk for both GI and mental health problems, as well as being associated with changes to the GI microbiome, suggests that the timing of this exposure (infancy to early childhood) coincides with the sensitive period for the maturation of each of these systems,” the authors wrote.
More research is needed, but Tottenham and Callaghan believe their study helps fill an important gap in the literature.
“Animal studies tell us that dietary interventions and probiotics can manipulate the gut microbiome and ameliorate the effects of adversity on the central nervous system, especially during the first years of life when the developing brain and microbiome are more plastic,” Callaghan said. “It is possible that this type of research will help us to know if and how to best intervene in humans, and when.”
Callaghan and Tottenham are working on a larger study with 60 children in New York City, New York, to see if their findings can be replicated. They expect the results later this year.
The study was supported by the National Institutes of Mental Health, the Dana Foundation, the American Australian Association, and the National Health and Medical Research Council of Australia.
[contentblock id=9 img=gcb.png]




I’ve done a lot of research in this area. I find this very interesting. Thanks for the info!
Yes, I can confirm that this is true. Thanks for posting!